Analytical Laboratory Management Practice in (GLP) Site
- Published on: Oct 27, 2017
The analytical laboratory in a pharmaceutical industry plays one of the most critical roles in ensuring quality products are built into strict specifications and supplied to its customers with no questionable safety, purity, efficacy issues. That is why regulatory agencies inspect this area with proper diligence to make sure plants are operating under stringent GLP (Good Laboratory Practice) and GMP (Good Manufacturing Practice) guidelines. Therefore, managing an analytical laboratory by expert hands is significant to achieve these regulatory and product quality goals.
A typical GMP laboratory management practice involves personnel training as applicable to the job function; managing hazardous materials; creating procedures (SOP) for sample handling and testing; designing laboratory facilities, handling and storing equipments and related systems as per manuals; creating a practice for calibration and maintenance of laboratory equipment; controlling and maintenance of reagents, reference standards, buffers, microbial cultures, culture media and biological indicators (BI); monitoring and controlling of the microbiology laboratory environment; documenting test results into records etc.
The primary roles of a GLP analytical and microbiology laboratory at a GMP site include testing of pharmaceutical raw materials, in-process and finished products, which are intended to be distributed into a marketplace. Broadly speaking, the test specimens rang from raw materials, regulatory starting materials, intermediates, active pharmaceutical ingredients (API), in-process materials, drug products, biologics and medical devices.
210 SOPs, 197 GMP Manuals, 64 Templates, 30 Training modules, 167 Forms. Additional documents included each month. All written and updated by GMP experts. Checkout sample previews. Access to exclusive content for an affordable fee.
As a good management practice the analytical and microbiology laboratories should be built separately into designated areas with limited access and should be maintained in a clean and organized state. Practices should be established at each GMP site to assure laboratory housekeeping is maintained. Work surfaces in the microbiology laboratory (e.g., benches, bio-safety cabinets, unidirectional airflow units) should be cleaned, organized and disinfected prior to and after use. Those disinfectants should be chosen which are effective in cleaning the expected types of organisms.
Laboratory equipments should be maintained in a clean state and should be stored in a manner that prevents contamination. Incubators, refrigerators, ovens & water baths, used in the microbiology laboratory, should be cleaned and maintained according to an approved schedule.
Laboratory instruments should be calibrated upon installation and thereafter, according to an approved schedule and be used within the calibration period or calibrated upon use.
Laboratory facilities and equipment should be qualified. Automated laboratory equipment and computer-related laboratory systems should include validation of the computerized System.
Laboratory processes (e.g., sterilization and depyrogenation) should be validated. Equipment and utilities (e.g., vacuum, compressed air, gases) used should be properly designed, commissioned and/or qualified.
Laboratory water systems should also be qualified for their intended use. The water system should be maintained, monitored on a routine basis and must be suitable for use for the specified test method or test material preparation. In addition, the water system in the microbiology laboratory must, at a minimum, meet the quality attributes for purified water.
Non-compendial test methods used for product release testing and stability testing should be validated to the established standard in place when the method was developed. The suitability of all test methods used should nevertheless be qualified under actual conditions of use and documented.
All test methods should be maintained under change control. Other methods, such as in-process test methods, should be validated as specified by approved procedures.
Personnel performing testing and personnel approving test results should also be trained and qualified.
Biological, toxic, and hazardous waste materials should be handled according to local, regional, and/or national guidelines as well as environmental health and safety (EHS) guidelines.
A sample handling system should be in place and include provisions for sample receipt, proper sample labeling and sample log-in; prevention of sample loss, sample mix-ups and contamination; verification that information on the sample label matches the accompanying document submission; identification of potent, toxic or hazardous compounds requiring special precautionary measures; sample storage at room temperature unless otherwise indicated; tests performed within a defined time period after sample receipt; investigation of sample mix-ups or contamination; sample retention until all tests are completed and there is a determination as to whether a result is valid or invalid; and sample destruction or disposal. Controls for preventing cross contamination should be available and implemented.
Reference standards used for testing production materials, actives, drug products and medical devices should be obtained or established, used, controlled, maintained and approved according to written procedures approved by the site quality assurance.
Laboratory materials for testing, such as reagents, buffers, reference standards, microbial cultures, microbiological indicators and culture media should not be used beyond their Expiration Dates. Expired materials should be discarded promptly. An investigation should be conducted if expired materials are used in error.
The identity of microbiological control cultures, when purchased from sources other than American Type Culture Collection (ATCC) and National Collection Type Culture (NCTC), should be verified to, at least, the genus and species level.
Every sterilized batch of media should be tested for growth promotion, sterility and pH after sterilization.
Glassware should be controlled and cleaned in a manner that ensures the glassware is suitable for its intended use. Glassware used in microbiological tests should be sterilized and/or depyrogenated, when required, using validated methods. Single use materials (e.g., plastic) should be disposed of after use.
Laboratory Records should be maintained as per site SOP. Any Out-of-Specification (OOS) result or questionable result should be investigated and corrective and preventive actions should be identified.
Records should be maintained for each sterilization/ depyrogenation load including date and time of sterilization/depyrogenation; identification of person performing sterilization/ depyrogenation activities; identification of all equipment and components in the load; cycle identification; sterilization/depyrogenation Batch Number or run number; documentation of the review of sterilization/depyrogenation cycles, including indication of pass/fail status, initials, and date; and sterilization/depyrogenation records retained according to site retention policies.
The Use of contract testing laboratories should be approved by the quality assurance and should be conducted according to a GMP quality agreement.
Related Posts
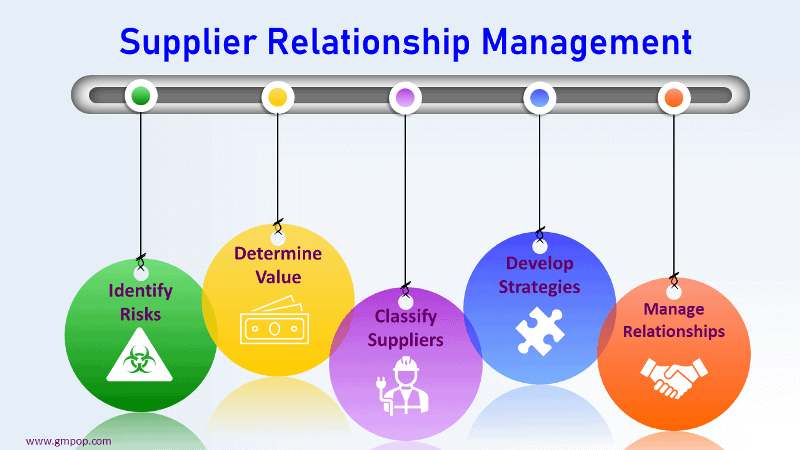
Raw Material Supplier Approval in GMP
Quality Planning at a Medical Device Processing Site
Quality Agreements with Third Party Manufacturer