How to process packaging and labelling for clinical supplies
- Published on: Nov 09, 2021
I. Introduction
Packaging, labelling, quality assurance and distribution of clinical supplies (drugs, biologics and devices) and regulatory stability supplies are regulated by Good Manufacturing Practice (GMP) and/or applicable ISO or EN Standards. For Medicinal Devices, compliance with EN 4600, and 21 CFR 820 need to be adopted.
II. Standard requirements
A. Quality Management
The Quality Assurance System designed, set up and verified by the manufacturer shall be described in writing, taking into account the GMP principles applicable to investigational products. In the case of devices EN46001, and 21CFR 820 is applicable.
Some of the production processes for investigational products that have no marketing authorization may not be validated to the extent necessary for a routine production operation. The product specifications and manufacturing instructions may vary during development.
Packaging and labelling operations for investigational products are often complex and are performed in accordance with specific requirements. These operations are of paramount importance for the integrity of clinical trials. For this reason, self-inspections or independent quality audits are an integral part of the Quality Assurance System.
210 SOPs, 197 GMP Manuals, 64 Templates, 30 Training modules, 167 Forms. Additional documents included each month. All written and updated by GMP experts. Checkout sample previews. Access to exclusive content for an affordable fee.
B. Organization and Personnel
The people responsible for releasing clinical supplies shall be organizationally separate from those responsible for producing those supplies.
All production operations shall be carried out under control of a clearly identified responsible person(s) nominated by line management. If necessary according to national law, the responsible person(s) shall be known to and/or be approved by the relevant national authority.
A distinction is drawn between processing and packaging/distribution activities when defining the QA unit with batch release responsibility. The QA unit at the development site which has responsibility for formulation and specification development is responsible for Quality Assurance release of the dosage form no matter where processing occurs. Responsibility for these batch release functions may be delegated to another QA unit. Packaging and distribution can be regarded as independent of the dosage form characteristics (with the exception of storage conditions and shelf life), and therefore, the Quality Assurance unit at the site where packaging and distribution occurs is responsible for release of packaged lots.
All personnel involved in manufacturing of products for clinical trials shall have competence and training within their area of responsibility and knowledge of GMP and/or EN46001 (for devices) as applicable.
There shall be written job responsibility descriptions, curricula vitae for key personnel, and up to date and approved organizational charts, training programs and individual training records for all personnel involved in GMP regulated activities.
When work is shared between intra-company sites or when it is contracted to a third party, a written agreement is prepared that captures the essential information required for the work to be successfully completed. This written agreement can take the form of a site-to-site specific agreement covering all operations or a job specific agreement. The agreement is prepared in advance of the work being conducted by the involved units at each site and is reviewed by the appropriate Quality Assurance (QA) unit(s) and approved by the appropriate manufacturing units.
C. Facilities and Equipment
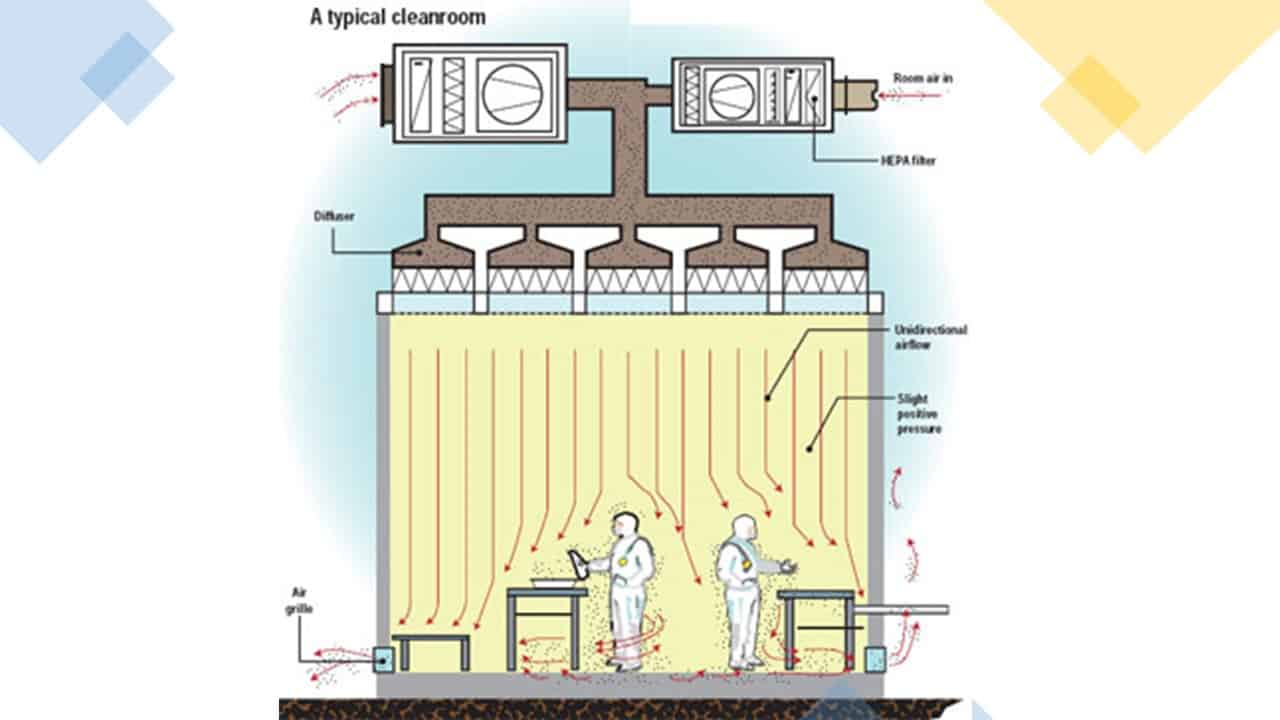
Facilities shall be maintained according to written instructions, and be suitable for the operations carried out in them.
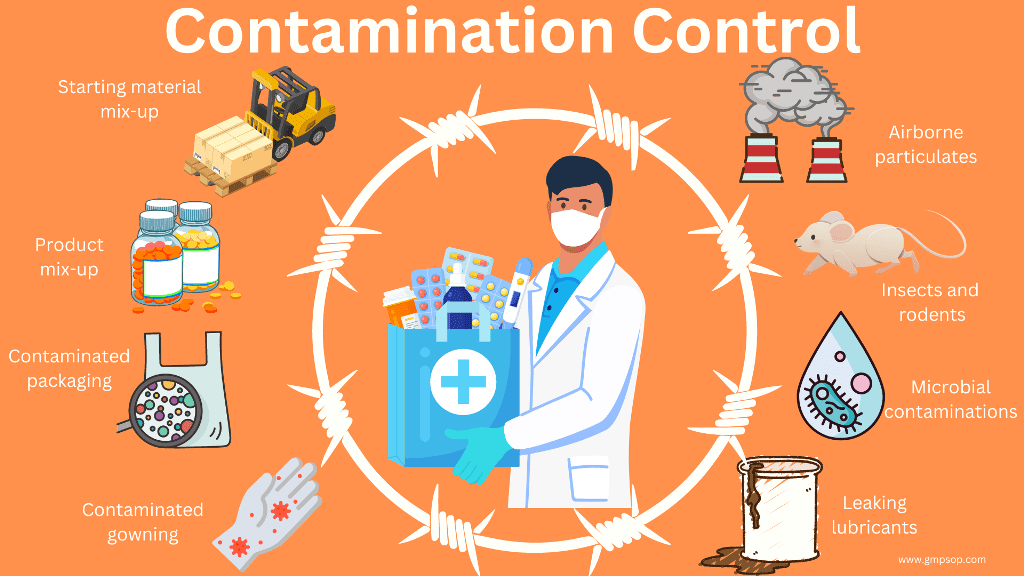
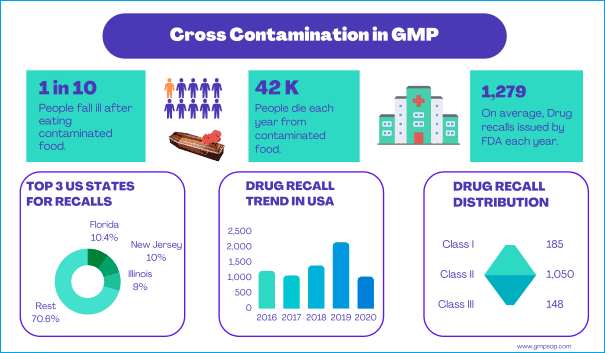
During manufacture of investigational products, it may be that different products are handled in the same area and at the same time. Appropriate procedures must be in place to minimize the risks of contamination, including cross-contamination and accidental mix-ups.
Investigational materials are not normally manufactured or packaged in product dedicated facilities. Because the toxicity of the material may not be fully known, evidence of effective cleaning must be obtained and facilities and equipment not used again after manufacture until effective cleaning has been verified. Additional precautions may be necessary for highly toxic materials.
Critical equipment, systems and facilities used in manufacturing shall be maintained according to written instructions. Facilities and utilities should be validated according to written protocols to demonstrate that they perform as intended. Equipment use, maintenance and performance checks shall be documented. In addition, measurement equipment critical to the process shall be calibrated regularly using traceable, certified standards, according to written instructions and the results must be documented.
For sterile products, validation of sterilizing equipment shall be to the same standard as for marketed product. While hand filling and sealing may be done on small-scale batches, it presents great challenges to sterility assurance. Enhanced attention shall be given to quality assurance of products produced by hand filling and sealing.
D. Documentation
1. Order (Request)
The order may request the processing, packaging or shipment of a certain number of units. Orders may only be submitted by authorized company personnel to an authorized provider of investigational product. Appropriate order forms should be in writing, formally authorized and precise enough to avoid any ambiguity.
2. Specifications
Specifications for starting materials, primary packaging materials and intermediate and bulk products should be established and approved by a responsible person prior to the use of the lot in clinical studies. Specifications shall be based on scientific data, the technology used, and the regulatory and pharmacopoeia requirements.
3. Manufacturing Formula and Processing Instructions
Manufacturing formula and processing instructions may be allowed, but allowance must be made for any possible repercussions on stability and on bio-equivalence between batches of finished products.
4. Master Documents
A master processing and packaging document may not be required, but for each manufacturing operation there must be clear and adequate instructions and written record. Systems or procedures shall be in place to ensure that the correct formula version is supplied.
5. Processing and Packaging Batch Records
Processing and packaging batch records shall be kept in sufficient detail for the sequence of operations, the equipment used, and the personnel who performed the operations to be accurately traced back. Original batch documents and relevant validation documents supporting processing or packaging of clinical supplies are archived at the site of processing or packaging.
6. Packaging Instructions
Packaging and labelling of investigational products are likely to be more complex and more liable to errors (which are also harder to detect) than with licensed products when “blinded” labels are used. Procedures such as label reconciliation line clearance, etc. and the independent checks by personnel performing quality control tasks shall be intensified accordingly.
Packaging instructions are based on the order and medical protocol. Batches of investigational products may be subdivided into different packaging batches and packaged in several operations over a period of time.
The number of units to package should be specified prior to the start of the packaging operations, considering also the number of units necessary for carrying out quality controls and the number of samples to be kept. Reconciliation should take place at least at the end of the packaging and labelling processes.
7. Labelling Instructions
Labels on the IMMEDIATE container should include the following:
i) Name and address of the company site producing or distributing the packaged supplies. If the company name/address cannot appear on the label (i.e. some trials for consumer products), traceability between the distributor name/address on the label and the company site must be documented.
ii) Batch/lot and/or code number to identify the contents and packaging operation
iii) Storage conditions and precautions if space permits. For small containers this information may be displayed on the outer container.
iv) Appropriate caution statement(s) as required by applicable regulations.
Unless it is determined that their inclusion would un-blind the clinical trial, the following items should also be present
v) Product identifier and strength
vi) Pharmaceutical dosage form and quantity of dosage form
Labels on the OUTER container should include the above mentioned items as well as additional information as deemed necessary or applicable. For example:
i. Directions for use or reference to an enclosed leaflet or requirement to take as directed by the physician
ii. The trial subject identification number
iii. Protocol title and/or protocol number
iv. Expiry or re-test date of the supplies (unless this is tracked by an appropriate system)
Information related to the Centre (such as Investigator name, Centre Number) when mandatory for a country should be printed on labelling affixed to the outer container.
The location to which the specific supplies are shipped shall be tracked by an appropriate system.
In the case of an expiry or re-test date extension, an additional label may be affixed to the investigational product. This additional label should include the new expiry or re-test date and repeat the batch number. It may be superposed on the old expiry or re-test date, but not on the original batch number.
i. A copy of each type of study specific label shall be kept in the batch packaging record.
ii. Approvals, representing compliance with protocol and regulatory requirements shall be documented.
8. Product Specification File
All the information necessary to draft the detailed written instructions on processing, packaging, quality control testing, batch release, storage and/or shipping conditions shall be referenced in a Product Specification File. This Product Specification File shall be continually updated, ensuring appropriate traceability to the previous versions (The information in the files supporting the US IND are essentially equivalent to the information in the Product Specification File).
9. Device Master Record
A Device Master Record containing all necessary information to document the performance and configuration characteristics defined for a medical device shall be established. This Device Master Record shall be continually updated, ensuring appropriate traceability to the previous versions.
Specifications (for starting materials, primary packaging materials, intermediate and bulk products and finished products), manufacturing formula and processing, packaging and labeling instructions may be changed frequently as a result of new experience. Each new version shall be approved by a responsible person, take into account the latest data, and refer to the previous version so that traceability is insured. Reasons for changes shall be recorded.
11. Document Retention
Batch records shall be retained in accordance with the Retention Schedule or according to national requirements, whichever is longer. Order forms are considered part of the batch documentation.
E. Production
1. Starting Materials
The consistency of production is influenced by the quality of the starting materials. Their physical, chemical and, where relevant, microbiological properties shall therefore be defined, documented in their specifications and controlled.
Specifications for the Active Pharmaceutical Ingredient (API) shall reflect the current state of knowledge.
Specifications for both the active pharmaceutical substances and non-active substances must be reviewed in the event of a process change or change in supplier.
Detailed information on the quality of the components shall be available in order to recognize and assess the impact of any variation on production.
2. Manufacturing Operations
During the development phase, validated procedures may not always be available. Provisional production parameters and in-process controls shall be set based on the knowledge and experience of key personnel. Where some steps in the process, such as mixing, have not been validated, additional in-process information (observations and monitoring results) should be recorded in batch documents. Additional quality control testing of investigational products may also be necessary.
Investigational products must be appropriately identified at all stages during manufacturing.
Reconciliation is an essential part of the control of the manufacturing operation. Reconciliation is the comparison of the mass of material that is used in a process step to the mass of material accounted for at the end of a process step (the sum of product, waste, samples, measured loss etc.). Material reconciliation should be calculated at the end of significant process steps and any abnormal discrepancy investigated.
Assurance of sterility for sterile investigational products shall be no less than for marketed products. Sterilization in the final product container is the preferred process where the nature of the formulation permits, or as required by regulations. Aseptic processing, if necessary, must be validated by media fills. The media fills must accurately represent the production process to be used in the manufacture of clinical supplies. The integrity of any container/closure system used for sterile investigational products shall be suitably validated.
3. Principles Applicable to Comparator Drug
In studies where an investigational product is compared with a marketed product, attention shall be paid to ensure the integrity and quality of the comparator product (final dosage form, packaging materials, storage conditions, etc.). If significant changes are to be made to the product or primary packaging material, tests and/or documentation shall be available to provide assurance that these changes do not influence the original quality characteristics of the product.
The expiry or review date stated on the original package has been determined for the dosage form in that particular package and may not be applicable to the product where it has been repackaged in a different container. It is the responsibility of the sponsor, taking into account the nature of the product, the characteristics of the container and the storage conditions to which the article may be subjected, to determine a suitable expiry or review date. Such a date is not later than the expiry date of the original package.
4. Radioactive Investigational Products
Investigational products containing radio labelled material shall be produced in suitable facilities according to GMP guidelines and applicable radiological safety requirements.
Where normal quality assurance release procedures cannot be followed, a written protocol shall be approved which details all production and quality control data to be considered before the investigational product is released. The QA unit will approve this protocol before the investigational product is manufactured.
5. Randomization Code
Procedures shall describe the generation, distribution, handling and retention of any randomization code used for packaging investigational products. Responsibility for generation of the randomization code rests with the clinical supply logistic unit unless local regulations dictate otherwise (for example in Japan).
6. Blinding Operations
A system shall be implemented to allow for a proper identification of the ‘blinded’ products. This system, together with the randomization code and randomization list shall allow proper identification of the product, including any necessary traceability to any codes and batch number of the product before the blinding operation.
Particular attention must be paid to the appearance of clinical supplies manufactured at different development sites or at the same development site at different times if the supplies are intended to be used in the same blinded clinical study. This is to ensure that the clinical supplies are sufficiently identical to not compromise the blinding of the clinical study.
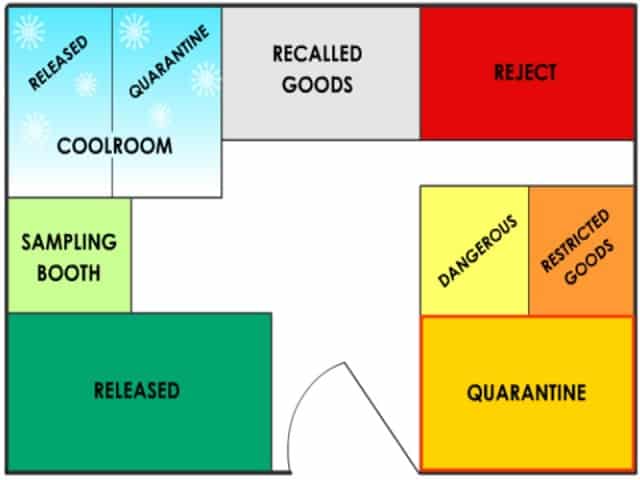
7. Storage Conditions
Investigational products must be stored securely under the labeled storage conditions to assure product stability in a manner designed to avoid mix-ups with other products. The development site is responsible for providing information on storage/shipping conditions for the dosage form and packaged clinical supply.
8. Retained/Archive Samples
Retained/Archive samples, of clinical supplies are stored at the site of processing and/or packaging. Additional retained samples of each test batch (sufficient to perform release tests required in the NDA at least three times) are required for bioavailability and bioequivalence (BA/BE) clinical study supplies. These are to be retained at the clinic site or an appropriate third party facility.
9. Testing
Laboratory testing of processed lots will normally be conducted at the development site responsible for a drug candidate development, no matter where the supplies are manufactured. Laboratory testing of packaged lots will normally be conducted at the site responsible for packaging. Appropriate tests may be conducted at the site of processing or packaging with the approval of the responsible QA unit (for example cleaning validation/verification tests, final packaged identification tests etc.).
F. Release of Investigational Product to Clinic Sites
Delivery of investigational products requires multiple approvals. The first approval is based on the approval of the batch record and the conformance of the results of the quality control tests carried out with established specifications. This release is given by the QA unit. Subsequent approvals assure that legal and regulatory commitments have been met for the shipment of investigational product.
1. Quality Assurance
Drug substances and investigational products shall be tested by appropriately validated analytical methods. Primary data obtained from testing of each bulk and packaged investigational product and each component of the lot shall be in accordance with the Retention Schedule or according to national requirements, whichever is longer.
Prior to Phase III, drug substance, excipients, drug product containers and closures used in the preparation of investigational products shall be evaluated and released by the QA unit prior to release of the investigational product for use in clinical studies. For Phase III and after, drug substance, excipients, drug product containers and closures used in the preparation of investigational products must be evaluated and released by the QA unit prior to use in manufacturing.
As processes may not be standardized or fully validated, in-process and end product testing takes on more importance to ensure that each batch meets its specification.
The QA unit shall especially pay attention to the compliance with specifications, which bear on the safety and efficacy of medicinal products, namely:
i) Accuracy of the therapeutic or unitary dose (e.g. homogeneity, content uniformity)
ii) Release of active ingredients (e.g. dissolution time)
iii) Estimation of stability if necessary in accelerated conditions, determination of the preliminary storage conditions and shelf life of the product.
There shall be a check on the similarity of “blinded” medicinal products (including packaging) using appropriate methods.
Samples of each batch of product (or drug substance) shall be retained under the responsibility of the manufacturer or importer, which released the batch for use. They shall be kept in the primary container used for study or in a suitable bulk container under the recommended storage conditions for the product (or drug substance). Samples are kept for 15 years from the time of processing or packaging (as appropriate) unless a shorter time is justified by the stability of the investigational material. If the investigational product is not stored in the package used for the study, stability data shall be available to justify the shelf life in the pack used.
2. Product Release
Product release is often carried out by QA in two stages, before and after final packaging:
i) Bulk product assessment: it shall cover all relevant factors, including production conditions, results of in-process testing, a review of manufacturing documentation and compliance with the Product Specification File or Device Master Record (or IND) and the Order.
ii) Finished product assessment: it shall cover, in addition to the bulk product assessment, all relevant factors, including packaging conditions, results of in-process testing, a review of packaging documentation and compliance with the Product Specification File, or Device Master Record (or IND) and the Order.
Release of investigational products, including batch documentation and independent quality assurance staff appropriately trained in quality systems, GMP and specific clinical and regulatory requirements shall carry out quality controls. In the EU a Qualified Person as referred to in Article 17 of Directive 75/319/EEC should carry out this task.
3. Free Movement between company sites
Since investigational products are released by appropriately qualified company staff at one site, subsequent analysis after shipping to other sites is not required for final, label, packaged clinical goods, as long as documented evidence is available that appropriate analysis and release procedures have been conducted and appropriate shipment and storage controls are in place. When bulk investigational product is being shipped to another qualified company site, an identification test is typically performed prior to the release by QA of the final packaged supplies to the clinic.
G. Distribution and Return
Shipping, return and destruction of unused products should be carried out according to written procedures. The distribution of clinical supplies to clinic sites is governed by GMP and GCP requirements.
1. Shipping
a. Shipping of investigational products is conducted according to orders given by the Sponsor, or their designee in the shipping order.
b. The packaging should ensure that the medicinal product remains in good condition during transport and storage at intermediate destinations. Any opening of, or tampering with, the outer package during transport should be readily discernible.
c. Systems shall be in place to assure that shipments are delivered to the correct addressee. Investigators should document the receipt of shipments.
d. A detailed inventory of the shipments made to the Market Company or the clinical investigation site shall be maintained by those making the shipment. It should particularly mention the addressees’ identification.
e. Transfer of investigational product from one trial site to another should remain the exception and be carried out in accord with applicable regulatory requirements.
2. Returns
a. Investigational products may be returned to clinical supply group control and re-released for distribution under conditions defined by the clinical supplies group which are specified in written instructions and approved by the responsible Quality Assurance unit.
b. Investigational products returned to clinical supply group control shall be clearly identified and stored in a dedicated area. Inventory records of returned products should be kept.
3. Destruction
a. The sponsor is responsible for the destruction of unused investigational products. The destruction can be carried out at the investigator site, hospital pharmacy or by the manufacturer, but shall always be under the authorization of the sponsor.
b. Recording of destruction operations shall be carried out in such a manner that all operations may be accounted for. The sponsor should keep the records.
c. If the manufacturer is other than the sponsor and is requested to destroy the products, he shall deliver a certificate of destruction or a receipt for destruction to the sponsor. These documents shall clearly identify the batches involved and the actual quantities destroyed.
H. Contract Manufacture and Analysis
If clinical supplies are manufactured or tested by a third party outside the company, there shall be a written agreement that clearly establishes the responsibilities of each party.
The written agreement must clearly state, among other provisions, that the investigational products or devices are being used in clinical trials. Cooperation between the contracting parties should be very close.
Authorized personnel shall check that the GMP and EN 46001 levels are in accordance with company methods/specifications and the legal demands. Normally this shall be performed by audits at the site.
I. Quality Audits or Self Inspections
There shall be operational programs of self-inspections or quality audits at all units involved in the production of investigational products. Designated competent persons shall perform the inspections and audits in an independent and detailed way.

Author: Kazi Hasan
Kazi is a seasoned pharmaceutical industry professional with over 20 years of experience specializing in production operations, quality management, and process validation.
Kazi has worked with several global pharmaceutical companies to streamline production processes, ensure product quality, and validate operations complying with international regulatory standards and best practices.
Kazi holds several pharmaceutical industry certifications including post-graduate degrees in Engineering Management and Business Administration.
Related Posts
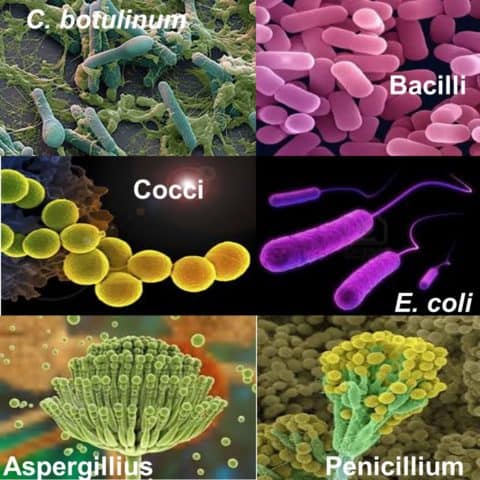
Overview of microorganisms found in production area
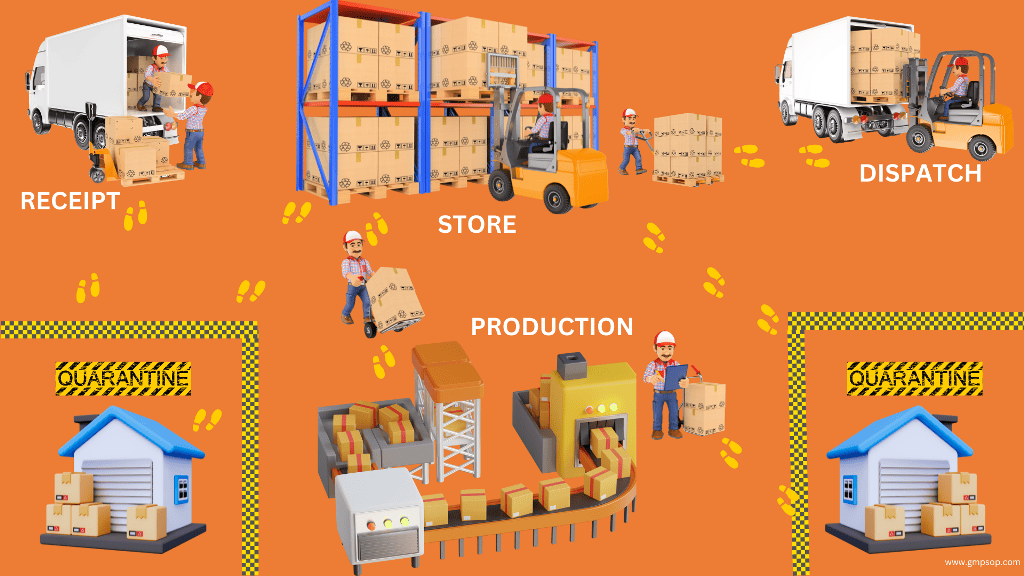
Warehouse material handling for pharmaceutical industry
Basic Overview of Contamination Control in GMP Facility