Guidance Summary 111 - 120
Guidance 111 Summary - Microbiological Testing in Cleaning Validation for APIs and Drug Products
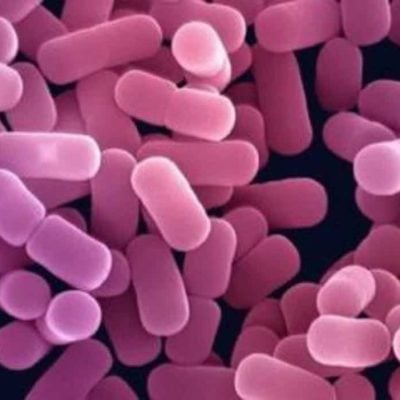
This document describes the rationale and recommended microbiological methodology for consideration during cleaning validation of product contact surfaces for Active Pharmaceutical Ingredients (APIs) and drug products.
Microbiological cleaning validation for product contact surfaces for drug products and the final stage of drug substances is advisable when the surfaces are not sterilized and water is used as a final rinse. When cleaning validation microbiological sampling is required, a final purified water (PW) or water-for-injection (WFI) rinse sample of product contact surfaces following the cleaning procedure is the preferred sample collection method. Alternatively, if a water rinse sample is not practical, then direct sampling (e.g. contact plates or swabbing) of the product contact surfaces may be used.
If surface sampling is needed, sterile swabs saturated with a sterile diluent such as Sterile Water for Injection or Sterile Saline Solution are used. The following sampling guidelines and associated limits are recommended.
For manufacturing equipment for non-sterile drug product and the final stage of drug substance where applicable: Final Purified Water rinse samples – Recommended limits should be based on preliminary or historical studies and action limits should take into consideration the microbiological limit of the rinse water, for example, not to exceed 100 cfu/ml (USP <1231> and EP “Water, Purified”). Drug substances using other than USP Purified Water must comply with site standards for water used as the final rinse.
Guidance 112 Summary - Overview of Trending of Environmental Monitoring Data for Aseptic Processing
How should environmental monitoring data be trended to assure microbiological control of aseptic processing areas?
This article establishes the need for trending of environmental monitoring data and gives recommendations on aspects of trending such as categorization of data, frequency of trending, trend definition and content of trend reports.
From a microbiological perspective, this means review of environmental monitoring (EM) results from each batch supplemented with periodic review of EM data over extended periods of time.
EM data in isolation provides a snapshot of microbial control at a discrete time point, but does not provide information on adverse trends that may be developing.
How often should trend data be reviewed? For example, it may be sensible to examine Grade A and B data for both short and long term trends while analysing Grade C and D data only for long term trends.
The easiest form of trending is to consider a certain number of alert level excursions equivalent to an action level excursion. While alert level excursions will show adverse trends in the short term, more advanced statistical treatment is required for longer-term data analysis.
Once the upper control level is established, it can be compared to the percentage of EM data points that do not conform to the chosen attribute
Guidance 113 Summary - Packaging System Integrity for Sterile Medical Devices
The microbial barrier properties of the materials should be determined by comparing the extent of bacterial or particulate penetration through the material with the original challenge.
Critical factors that affect packaging system integrity for sterile medical devices include, and are not limited to:
- Packaging components composition, dimensions, coatings, and critical defects;
- Sealing/packaging operation variables of time, temperature, pressure (seal force), gas flow rates, torque limit, and energy level/frequency (radio frequency/ultrasonic);
- Processing variables of packaging components including washing, drying, siliconization, and sterilization; and
- Final product processing, such as terminal sterilization.
Sealing equipment commissioning and/or qualification should include and not be limited to:
- Verification that the sealing equipment is installed according to design criteria;
- Verification of mechanical operation (e.g., valves, hydraulic vacuum pumps, heating elements);
- Identification of utilities and instruments and elements (I/Es);
- Calibration of I/Es;
- Testing of alarm systems; and
- Verification that equipment operates properly throughout the Normal Operating Ranges.
Guidance 114 Summary - Preventing Cross Contamination
Facility Design should include consideration of, and not be limited to, the following items:
- Room and equipment layouts that minimize potential cross contamination of products (e.g., use of airlocks);
- Use of closed processing equipment;
- Air quality, airflow requirements, and air re circulation controls;
- Product and material flow;
- Personnel flow and gowning requirements;
- Collection, transportation, and storage of waste;
- Drainage systems; and
- Cleanable continuous, smooth, and non-porous floors, walls, doors, and ceilings with surfaces able to withstand repeated application of cleaning agents.
Dedicated Manufacturing Facility aspects include, but are not limited to:
- Dedicated building with dedicated entrances and exits for personnel and materials;
- Dedicated utility systems, including air handling;
- Dedicated personnel (i.e., no cross flow with other personnel after entry to the area);
- Dedicated materials (i.e., no cross flow after entry to the area); and
- Dedicated laboratories.
In-Process Sampling should be conducted according to SOPs designed to prevent cross contamination of the sampled material and other materials, intermediates, APIs, in-process materials, drug products, or medical devices.
Guidance 115 Summary - Prevention and Control of Fungal Contamination in Tablets
What steps can be taken to prevent and control of fungal contamination in tablets?
This document discusses the prevention and control of fungal contamination in tablets production to include: raw material and API testing, manufacturing processes, environmental monitoring, and final product testing.
Fungal contamination is most commonly introduced into a tablet via the following:
- Steps of the manufacturing process of the tablet where water is present (e.g., wet granulation, coating solutions).
- Contaminated raw materials, excipients or active pharmaceutical ingredients (API).
The microbial quality of the raw materials and APIs directly impact the microbial quality of the final tablet product. Fungal populations that may be found in these raw materials can contaminate the final tablet product.
The Total Yeast and Mold Count tests for raw materials and APIs in the tablet formulation are validated and tested according to compendial methods and/or internal requirements. Specific limits for fungal levels in raw materials and APIs are used to ensure that the microbial quality of the final dosage form will not be adversely affected.
During the manufacturing of a tablet, fungal contaminants may be introduced into the tablet via the water introduced into the process.
The holding times of the wet powder should also be validated with microbial/fungal considerations in mind. The validation of a holding time should be based on both time and temperature parameters. The longer the wet powder is stored, the greater the possibility the microbial quality of the tablet will be adversely affected.
Guidance 116 Summary - Sanitant Rotation in a Routine Sanitization Program
What are the expectations for industry for the inclusion of different sanitization agents within a routine sanitization program? Additionally, are there tangible benefits to routinely rotating sanitization agents? Finally, how is sanitant performance defined?
For the purpose of this discussion, the terms sanitization agent, sanitant, sanitizing agent, antiseptic and disinfectant are used interchangeably as all of these agents are primarily designed to reduce microbiological bioburden on applied surfaces.
The practice of rotating sanitization agents has primarily been based upon accepted wisdom that routine exposure to a single sanitization agent over time can promote the selection of microorganisms with increased resistance to antibiotic agents. This document discusses the current argument for sanitant rotation and provides points to consider in determining when the rotation of sanitants is beneficial as part of a routine sanitization program.
While development of resistance to sanitization agents is not scientifically supported, differences in innate resistance is a factor to consider in a sanitization program, including rotation of sanitization agents.
Of primary importance in any sanitization program is the proper selection of a chemical agent to reduce microbial bioburden.
Guidance 117 Summary - Sterilization or Depyrogenation Validation for Non Product
Preventive Maintenance (PM) Measures should include, and not be limited to, the following:
For Steam
- Calibrate instruments and elements (I/Es);
- Check operation of vacuum pumps;
- Clean chamber, steam traps and drains;
- Perform leak test of the chamber;
- Replace and integrity test vent filter;
- Verify the operation of safety devices; and
Sterilizer Monitoring and Control I/Es should be calibrated before the operational qualification (OQ) study and routinely according to a defined calibration schedule
For continuous belt depyrogenation tunnels, thermocouples should be fed into the tunnel (i.e., trailing thermocouples) in containers distributed across the belt, at least in the first and last rows of each load.
Custom Prepared BIs for moist heat sterilization or dry heat sterilization should be tested prior to use for survival time and kill time under the conditions in which they will be used. D-values and kill time required for complete inactivation of prepared BIs should be determined experimentally. BIs having high D-values and/or large spore populations can result in some survivors when using the overkill sterilization cycle.
Steam Sterilization OQ/PQ Studies should be performed and include, and not be limited to, the following:
- A minimum of three (3) temperature distribution runs on an empty chamber to confirm heating uniformity and identify the slowest-to-heat zone;
- Heat penetration runs on each different load configuration to identify cold spots, the effect of loading on thermal input, and the worst case load configuration.
Guidance 118 Summary - Unplanned Cleanroom Power Outage Time Limit and Recovery
Appropriate steps to be taken during and after an interruption of air supply to the aseptic processing area. Qualification studies should be carried out to define a time limit after which the controlled environment reaches or exceeds action levels for particulates, temperature, humidity, and pressure differential.
Qualification studies should be carried out to define a time limit after which the controlled environment reaches or exceeds action levels for particulates, temperature, humidity, and pressure differential.
Production loses from power outages can be minimized or eliminated by supplying critical equipment with power from generators, automatic transfer switches and uninterruptible power supplies.
Handling power outages to air handling systems is needed. Setting a time limit without supporting data will risk product contamination or the unnecessary destruction of sterile product.
Determination of a time limit consists of extensive environmental monitoring after the aseptic processing area power has been interrupted and the critical air handling systems viable particulates, viable quantitative (active) air and/or viable passive air (settling plates), and pressure differentials.
The Non-viable monitors and pressure differential monitors are the most sensitive monitors.
Non-viable particulate and viable microbiological air tests used to determine a power interruption time limit are quite similar to the qualification studies used to classify the area. The monitors are placed in the controlled area while the air handling system is operational. At time zero, power to the air handling system is shut down and the air is continuously monitored for a defined length of time.
Acceptance criteria for air quality tests should be no higher than the action levels employed during routine production.
Another key parameter in defining a power interruption time limit is the flow of air through the classified area. As in air quality tests discussed above, pressure differentials are monitored after the air handling system is shut down and the time measured until the differential reaches a predetermined acceptance criterion.
Guidance 119 Summary - Use of Sterilized Goggles Within the Aseptic Processing Area
The FDA has supported the use of sterilized goggles as supported within its’ Guidance document “Guidance for Industry – Sterile Drug Products Produced by Aseptic Processing”, published in September 2004. This guidance indicates that gown articles worn within the aseptic processing area should be sterilized and further specifies goggles as part of this sterile ensemble.
Validation documentation of the sterilization of these goggles needs to be reviewed and is available from certified vendors.
Any vendor that supplies re-usable goggles will need to have complete validation data readily available for review to support the goggles throughout its’ lifecycle if the goggles are cleaned and re-sterilized by the supplier. In some cases complete validation packages are available that document a sterilization compatibility program for their product, regardless of sterilization location, within specified sterilization parameters.
Goggles sterilized by ethylene oxide (ETO) must also have safety data available that verifies any remaining residual levels of ETO present in the goggles post sterilization is below established exposure limits for each sterilization cycle.
Re usable goggles are more cost effective over the long-term and numerous studies have been completed by goggle suppliers, evaluating the effects of repeat sterilization on goggle components.
While sterilization of the goggles is the focus of this bulletin, cleaning of the goggles is a potentially critical component for any re-usable goggle due to the direct ability to properly re-sterilize (e.g. ETO).
If reusable goggles are chosen, the decision to sterilize on site depends on the sterilization technology available, goggle component compatibility, and the commitment to develop, document and maintain an overall goggle sterilization program.
Guidance 120 Summary - What Is It Water Activity & How Does It Apply to Pharma Manufacturing
Water activity (aw) is defined as the ratio of product vapour pressure to pure water vapour pressure. It is a measure of the water available for chemical or microbiological activity within a product. Water activity is significant to the pharmaceutical industry in that it affects the quality of ingredients and finished product through their chemical stability, a reduced need for chemical preservatives, and a potential reduction in the need for microbial limits testing.
Microbial growth requires water. Water dissolves solutes within a viable cell and is required for metabolic function. When an (aw) value is associated with a micro-organism it serves as an indication of potential metabolic activity. While organism proliferation ceases below certain water activity levels, some species have the ability to adapt slightly and continue to grow at levels below their optimum range.
Molds can tolerate aw levels down to about 0.80. Microbiological growth at any level ceases at aw values of about 0.60. Thus, by controlling the water activity of products, the growth of microorganisms, when present, can be controlled as well.
The aw also has an effect on the chemical processes within a product or formulation.
Lowering the aw may increase chemical stability. Freezing, freeze drying, salting, syruping, and drying are preservation methods that take advantage of lowering aw. These methods either bind or eliminate the available water in a product. Ideally, water activity should be evaluated early in the product development process.
Low aw can be achieved by limiting the amount of water added to a product during formulation, driving off water, or binding remaining water.
Water is often used to dissolve product constituents. Different solutes provide different aw results.
The aw of a product may also be examined over time to support product stability. If water activity levels can be achieved and maintained below predetermined levels known to support growth, microbiological and chemical stability of products can be maximized and the potential exists for a reduction in routine microbiological testing.
